How to help people on open-source automated insulin delivery systems?
Aug 28, 2023
This month, Diabetes Canada released a fascinating publication discussing open-source closed-loop systems.
- The organization issued a comprehensive position statement, conveying a crucial message urging clinicians to actively support individuals utilizing do-it-yourself (DIY) automated insulin delivery (AID) systems.
- Additionally, they furnished a guide tailored for healthcare providers, offering them insights into effectively carrying out this support.
What's truly noteworthy is the unequivocal endorsement of these systems by the national patient organization of Canada, despite their lack of official approval and their off-label status.
Canada has maintained a leading role in the advancement of DIY AID technology, even witnessing endocrinologists actively assisting patients in configuring these systems.
To craft this position paper, two official committees meticulously reviewed the literature surrounding DIY AID systems.
To ensure accurate guidance, they enlisted the expertise of a Canadian lawyer.
For your reference, you can access the original papers here:
To commemorate the release of these seminal papers, two informative webinars were organized.
- One is tailored for healthcare providers and can be accessed through this link. Upon registration, the passcode is: diabetes_1.
- The second webinar is designed for individuals with diabetes and can be viewed on YouTube.
In this blog post, we will delve into the pivotal recommendations outlined in the position paper and the healthcare providers guide.
Our aim is to provide you with a comprehensive update in a concise manner.
Furthermore, we have integrated pertinent quotes from both webinars to enhance the discussion.
Key recommendations from the DIY AID Position Statement

1. DIY AID can be effective to help individuals with type 1 diabetes improve glycemic outcomes, while reducing the burden of diabetes management.
"We really feel, after reviewing the literature, that the risks of using DIY AID are no different than the risks of using any AID system. Pumps can fail, both commercial and DIY systems, and so all of the usual sort of sick day management and other things, is just part of our prescribing practices, whether we're prescribing an off label or a commercial system." - Dr Ilana Halperin, University of Toronto
2. Healthcare providers have an obligation to discuss all available treatment options that have evidence of benefit with individuals living with type 1 diabetes, including DIY AID options.
"We need to remember that diabetes is a do it yourself condition. From diagnosis we had people on high alert, potentiallly very harmful medication. That is also life-sustaining. We give them insulin. We give them a glucose monitor. We teach them some basics, and they have to do it themselves. And so DIY AID is just the next step in this pathway of doing it yourself. And so the review of the evidence and the ethics is quite clear that as healthcare practitioners, we have an obligation to inform people with diabetes of all evidence-based treatment options. And DIY is one of the evidence-based treatment options. I would argue that we now have enough data to say that AID in and of itself is the gold standard of care for diabetes, to allow patients to reach that target time and range without an excess of hypoglycemia and decrease the burden of living with diabetes. And DIY should be considered alongside other commercial options. The time to say, no, you can't do this, I'm going to be the gatekeeper because you don't have carbohydrate counting skills, or you have not done your blood work frequently enough, I think we really need to challenge those assumptions. Because it's the people that are struggling the most, that are likely going to get the most benefit from these AID systems." - Dr Ilana Halperin, University of Toronto, Canada
3. Healthcare providers should connect interested people with diabetes to trusted online, social media and in-person resources
"Healthcare practitioners should connect interested people with diabetes to trusted online social media and in-person resources but they're not obligated to build the systems for the patients. In fact it's best when patients build these systems on their own or using the support of the online community so they know how to troubleshoot it when things go wrong. [...] It's important to recognize that it's not the job of the health care professional to build the app for you. That is why it's called DIY. If you're using a commercial system you can call a 1-800 number if you're having technical support. If you're using a DIY system the technical support is your online community. However these online communities have grown so significantly that sometimes you can get better support at three in the morning because there's someone from Australia who happens to be on Facebook, then you can from the 1-800 numbers" - Dr Ilana Halperin, University of Toronto
"Do it yourself doesn't mean do it alone. In order to prepare people living with diabetes for a successful transition to using a DIY system, the community has created exceptional step-by-step directions as well as 24 h worldwide volunteer based support. If you direct them to the Looped Facebook group, it will direct them to the other resources. Full disclosure, I created that group. I started the group to help a handful of folks, and it's grown to over 31,000 people with diabetes, researchers, health care, providers, and supporters. Now the group is heavily moderated and very task-specific. So you don't have to worry about people getting distracted or given wrong information when they go in there." - Kate Farnsworth, founder Looped FaceBook Group, Canada
The HCP guide outlines trusted DIY AID online resources:
- Community support: Looped Facebook Group, Discord #WeAreNotWaiting (Invite Link)
- System specific information, education and build instruction: LoopDocs, OpenAPS, AndroidAPS (other links are: iAPS, Nightscout, Tidepool)
- Education: Artificial Pancreas e-book, Loop and Learn
4. Healthcare providers should continue to provide ongoing support and education to people with diabetes using DIY AID systems, including assisting with optimizing pump settings and coaching on the behaviours linked to decreasing glucose variability.
"We know that one of the reasons people don't use DIY AID is because they're worried their healthcare team doesn't support them. Our Diabetes Canada position paper makes a strong statement that for diabetes professionals who support AID meaning they're comfortable enough with insulin pumps and continuous glucose monitors and so they're ready to prescribe commercial systems, they should also be supporting patients using DIY. They're actually quite similar and we should support our patients autonomy and their ability to choose the system that's best for them in managing their complex chronic disease. But if your healthcare professional does not support DIY AID, maybe they can make a referral to a team that does. Perhaps they haven't had a patient before but they're willing to learn with you. Certainly I learned the most from my patients who are using DIY AID even before there were commercial systems available, such that once the commercial systems came along and became available in Canada I was able to take some of my early learnings and apply those to my patients using commercial systems. There's more similarities then differences between these different control algorithms so usually a practitioner who's comfortable with the general automated delivery system will be comfortable. You can also let them know, because maybe they don't know that the diabetes Canada position paper and Healthcare users guide has been published and that they can get lots of useful tips and tricks to help support you." - Dr Ilana Halperin, University of Toronto, Canada
How are DIY AID systems different from commercial AID systems?
DIY AID systems are as safe and effective as commercial AID systems, but there are differences.
To explain this, we will use the CARES paradigm.
Calculate
DIY AID systems modulate a preset basal insulin rate every 5 minutes based on the glucose prediction in the coming 5-6 hours.
- They take into account the insulin on board and the carbs on board, and adjust the preset basal insulin rate to bring the predicted glucose into the target range.
- Basal adjustments and automatic boluses are accounted for in active insulin or insulin on board.
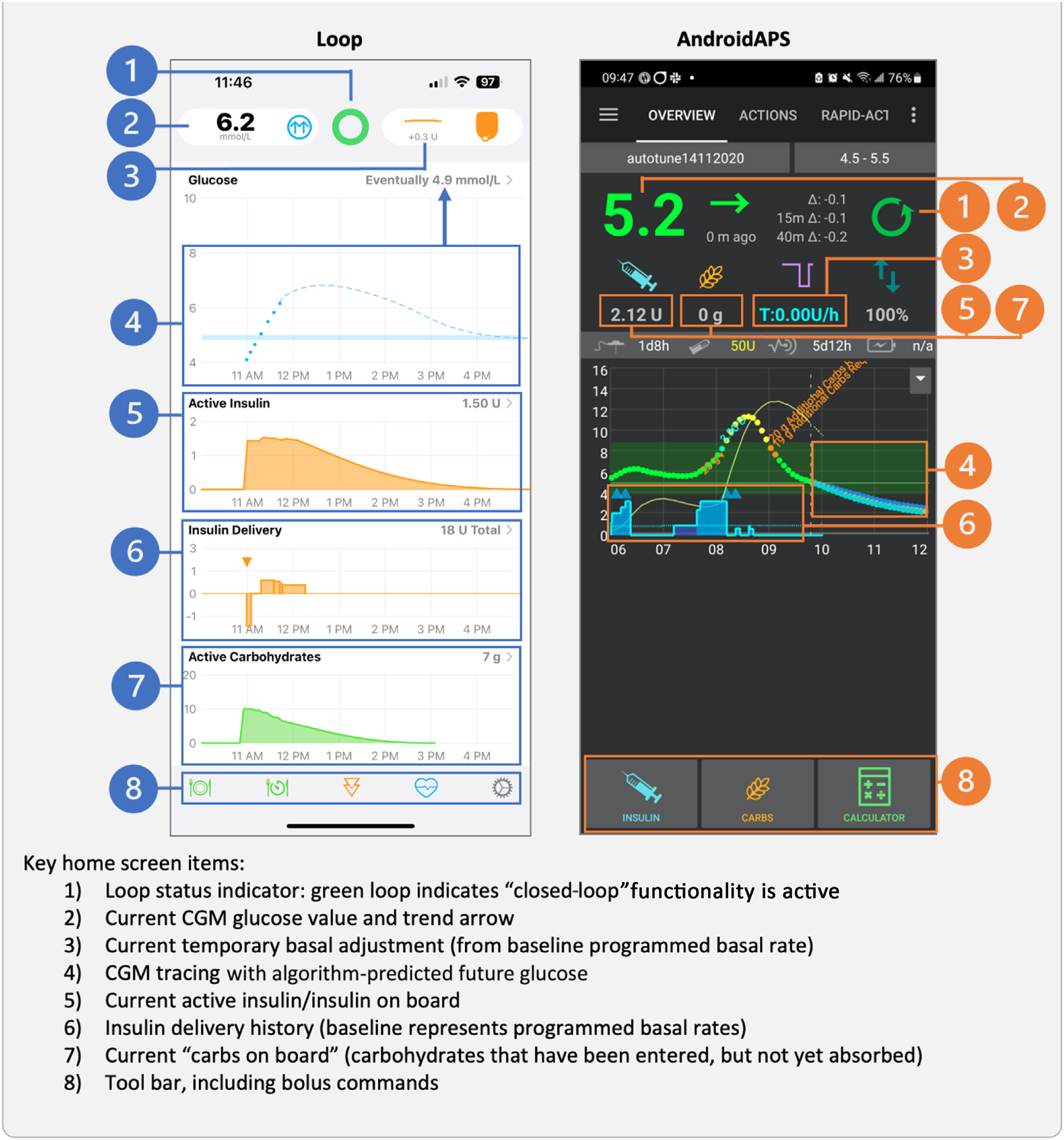
- You can follow the glucose prediction, the active insulin or insulin on board and the actual basal insulin delivery on the home screen of your app.
"I would really just encourage you, if you have someone coming in and using this [Loop or AndroidAPS app], ask them to show it to you and ask them to maybe explain which pieces of their home screen they look at. You're going to learn a lot through looking at that with people and and looking at lots of different scenarios. So they just have lunch, and so we're seeing this happening in real time on their Loop app. I think that's probably one of the most valuable educational pieces of getting comfortable with it." - Alanna Chambers, Registered Dietitian & Independent Insulin Pump Trainer Canada
It's important to understand that the eventual blood glucose showed at the end of the glucose prediction is not the real blood glucose you're going to have in 5-6 hours.
- The eventual blood glucose is the predicted blood glucose in 5-6 hours, but the algorithm will try to keep you in target by adjusting the basal insulin delivery every 5 minutes.
- So don't be alarmed if you are predicted to have a hypoglycemia in 5-6 hours, the algorithm will probably be able to fix this.
Adjust
In DIY AID systems, you can adjust
- basal rates (sometimes different basal rate profiles are possible),
- insulin sensitivity factor (which will have effect on the manual boluses and on the modulation of the basal insulin delivery),
- carb ratio,
- target value (or "correction range"),
- insulin model (duration of insulin action or active insulin time),
- delivery limits (max basal and max bolus)
- and suspend thresholds.
One key difference is that the DIY AID systems use insulin models that more accurately match how insulin works in the body!
They use a duration of insulin action of 5 or 6 hours, rather than an artificially short duration used in some commercial options like 2 or 3 hours.
It's recommended that people set up their DIY AID system and operate it in "open-loop" first.
That way they can evaluate and adjust their settings prior to enabling the closed-loop functionality to avoid inappropriate insulin delivery.
Especially when you change your duration of insulin action, other settings usually need to be adjusted at at that time.
Revert
When your phone is off, or when communication between your phone and the sensor and/or insulin pump is disrupted,
the system reverts back from "closed-loop" to "open-loop".
Insulin delivery will continue using the standard pump settings.
Users can manually revert to “open-loop” at any time.
They should consider this
- during illness and/or ketosis, when potential prolonged suspensions may create risk,
- and during periods of inaccurate glucose sensor performance.
When an infusion set or pod failure is suspected, users should monitor glucose and ketone levels, and administer manual corrective insulin.
If a manual injection is required via insulin pen/syringe, closed-loop functionality should remain turned off for the duration of the insulin action time since insulin-on-board calculations will not be accurate.
To be prepared for unexpected periods of “open-loop,” it's important to have accurate and safe standard pump settings
and have a backup plan for reverting to subcutaneous injections.
Educate
"Whether you're on commercial system or a a DIY system, settings have to change. We have to have overrides which we're going to talk about. You have to just change the settings because your physiology changes, your weight changes, people's insulin sensitivity changes across the seasons across the month. And so I think that's the key here is. It's not a one and done situation. It's a fantastic tool, but it's only as good as the underlying settings."
Ongoing education should be comparable to other AID systems.
The HCG guide provides 3 lists of key education points for DIY AID users:
- Self-management education points for DIY AID users
- Clinical considerations for optimizing DIY AID settings
- Exercise adjustment factors to consider with DIY AID systems
Because everything in DIY AID systems is so customizable, it is important to prioritize safety.
"I often do find that some patients like DIY AID because they're the type of people who live with diabetes that like to live on the edge of hypoglycemia. They're very, very preoccupied with having that tight time and range, and they can end up with more hypoglycemia than some of our commercial systems, because of that adjustable low, like kind of baseline and adjustable suspend threshold. So it's certainly always a shared decision-making conversation between my patient and me. When I say, you know, 4% low, I don't think you need to be 4% low, but then, otherwise I'm not 82% time and range. So we make a decision together. But these are some key safety settings to be talking about. [...] Loop has those guard rails now built in, too. So you can't set your system to be wildly, excessively aggressive. I mean, you can still be more aggressive. But there are some third rails." - Dr Ilana Halperin, University of Toronto
People with diabetes should be encouraged to prioritize setting optimization for minimizing hypoglycemia risk,
before fine-tuning to achieve a glycemic goals beyond the international recommended time in range.
You should also pay attention to the max basal, the max bolus and the suspend threshold.
- The maximum basal should be higher than the programmed basal rates to allow for effective temporary basal adjustments, but even experienced users do not set this to exceed more than 3 - 4 times their average hourly basal rate.
- The maximum bolus should not be set higher than a typical large meal bolus.
- The suspend threshold should be balanced between the risk of hypoglycemia and the risk of prolonged basal insulin suspensions.
Sensor
"Always making sure that they're not just saying, Hey, I'm on the system because I don't want all the alerts in the alarms with the commercial systems, and they shut everything off. It's like, hang on! Hang on! Let's make sure you still have your alarm on with your CMG, or your urgent low soon, because in some of those situations, no matter how much you think the system has your back, there are some times that you do need to intervene and still treat a low, so just an important double check can catch things sooner there." - Dr Ilana Halperin, University of Toronto, Canada
The list of compatible rtCGM devices continues to evolve as sensor technology advances.
It is important to be aware that with DIY AID systems, it is possible to
- extend the sensor life to longer than approved by the company,
- shut off urgent low glucose alerts
- and use FreeStyle Libre sensors as real-time CGM, which brings an extra layer of uncertainty with accuracy and reliability.
Users of DIY AID systems should be encouraged to
- perform a fingerstick glucose reading any time their symptoms do not match their sensor readings.
- use CGM low and high alerts, including snooze/repeat times, to prompt PWD to take action and problem solve when sensor glucose is reading in the hypo- and hyperglycemic ranges.
- If the sensor is not reading accurately, closed-loop functionality should be temporarily turned off until the sensor has been replaced.
Share
"How do I do this in my clinic? This is a question that a lot of people ask me. So I have a patient in front of me. They're still in "open-loop" and I talked them through their options. Today we have lots of patients in Canada who want to be tubeless, and they want AID. I'm often on Zoom, and if I'm in person with them, then I'm showing them those 2 links, the Looped Facebook group and the Loopdocs. And I'm putting it in the chat where I'm emailing it to them afterwards. I say to them, I'm your diabetes doctor, I'm not your tech support. I cannot build this app for you. But when you come back to clinic, make sure you're using some system that we can dig into the data together, and we can be sure together to optimize your settings. And then I describe that there's no helpline. There's no tech support with a 1 800 number. But you've got this Facebook group, and I trust it. And I think that that goes a long way. And the number of patients I've heard say to me "because you trust it doctor, I'm going to trust it too", goes a very, very long way." - Dr Ilana Halperin, University of Toronto
Sharing capabilities are available for CGM systems via manufacturer apps.
Healthcare providers may recommend that people with diabetes using DIY AID systems connect to Nightscout or Tidepool.
- Nightscout is an open-source solution developed by people with diabetes that provides browser-based visualization for DIY AID users.
- Tidepool is a free platform that allows DIY loop users to upload their glucose, carbohydrate, and insulin delivery data to their account and share their data with their clinician.
Here are some tips for using Nightscout
- Users will need to create a Nightscout account and follow the set-up instructions in the documentation for their specific system.
- Users can share their individual web address to share their data.
- To view reports from the real-time data home screen, click on the drop-down main menu (top right), and choose REPORTS. Select the data range you prefer, and check the glucose target. Don't forget to click on SHOW to generate reports.
- Most used reports are Distribution, Percentile Chart, Day to Day and Profiles.
- More information on Nightscout is available at: https://nightscout.github.io.

And here are some tips for using Tidepool
- Users will need to install the Tidepool Mobile app on their phone, create an account, and follow the steps on LoopDocs. CGM, insulin delivery, carbohydrate data, and notes
will sync without the need for an uploader. - To view Tidepool reports on a computer, the Chrome web browser must be used.
- If data is not visible at first, ensure the user has entered a note in their Tidepool Mobile app.
- Loop settings are not visible in the Device Settings report, since this information cannot be uploaded from Apple Health. To obtain device settings, ask users to show you or capture
screenshots of their device settings directly from their Loop app. - Most used Tidepool reports are Trends & Daily.
- For additional information on using Tidepool with Loop, including options to set up a clinic account, visit: https://loopkit.github.io/looptips/data/tidepool
Frequently Asked Questions
Concluding the HCP guide, a selection of frequently asked questions (FAQs) was incorporated, effectively highlighting the primary challenges faced by healthcare providers.
The authors adeptly addressed these obstacles and concerns, demonstrating thoroughness in their approach.
The extracted questions are presented below:
1. How is safety maintained when people are downloading “code” from the internet without regulatory approval?
The creators of these systems are individuals living with T1D or caregivers of T1D patients. Safety and hypoglycemia avoidance are paramount goals. Open-source materials specify that users assume the risk of building these systems and pledge to test all updates with volunteers. Individuals with diabetes (PWD) are encouraged to stay engaged with the community to stay informed about safety recommendations and advised to incorporate algorithm updates.
2. If a PWD has an adverse event (severe hypoglycemia, diabetic ketoacidosis) while using these systems, can I be found negligent/liable if I have supported them?
Managing T1D necessitates insulin therapy, inherently entailing risk of severe complications. HCPs are responsible for educating PWD and equipping them with skills to avoid such complications, regardless of insulin delivery method. The method, whether commercial AID, basal/bolus therapy, or DIY AID, carries equivalent risks. As of now, DIY AID has not been litigated in Canadian courts, but it's advised to recognize the common risks and prioritize HCP support and education for safe outcomes.
3. Can I refuse to support PWD using a technology I am not comfortable with?
HCPs confronted with unfamiliar territory should communicate its non-alignment with their expertise and refer accordingly. Nonetheless, diabetes-focused HCPs should strive to familiarize themselves with available treatments for T1D and T2D. While becoming an AID expert may be impractical for those with limited T1D cases, referral to more knowledgeable professionals is a viable option within provincial resources. Supporting DIY AID users should mirror support given to commercial AID users.
4. Is there a risk of using an out of warranty pump to deliver insulin?
All technology has inherent failure risks. In-warranty pumps are replaced by manufacturers, but this obligation expires post-warranty. Some manufacturers offer temporary loaner pumps. In provinces with shorter warranty durations compared to funding cycles, many PWD use out-of-warranty pumps, irrespective of their AID choice. A backup plan should be established for transitioning back to open-loop or MDI in case of pump or CGM failure.
5. How can I view the insulin and glucose sensor data from the PWD in my practice who are on DIY AID?
Nightscout, an open-source solution, provides browser-based visualization for DIY AID users, enabling retrospective analysis and remote monitoring to facilitate HCP interactions. Tidepool allows DIY loop users to share glucose, carbohydrate, and insulin data with their clinician.
6. What happens if the PWD does not have their phone or goes “offline”?
The algorithm utilizes Bluetooth communication between CGM, phone, and pump, thus continuous internet access isn't necessary for AID functionality. If the phone dies or is left behind, basal rates will continue insulin delivery. However, closer glucose monitoring is advisable as the system won't adjust to prevent hypo- or hyperglycemia.
7. What if CGM readings are inaccurate for a time period; how will this impact insulin delivery?
Similar to commercial AID users, PWD should perform fingerstick glucose readings if sensor readings don't align with symptoms. Utilize CGM alerts and set delivery settings appropriately to mitigate potential over- or under-insulin delivery. If the sensor inaccurately reads, disable closed-loop temporarily until sensor replacement. Third-party adaptors may introduce uncertainties in accuracy and reliability, warranting regular fingerstick checks.
In conclusion, the DIY AID Position Statement and the Healthcare Provider Guide provide invaluable insights into the realm of do-it-yourself automated insulin delivery systems.
Addressing critical barriers and concerns, these documents shed light on the potential benefits, responsibilities, and challenges that healthcare professionals and individuals with diabetes face in navigating this innovative landscape.
By fostering understanding, offering guidance, and emphasizing the importance of continued support and education, these resources empower both patients and practitioners to make informed decisions.
To further enhance your grasp of this evolving field,
we encourage you to download our comprehensive overview that compares 10 closed-loop systems,
ranging from DIY AID to commercial options.
By staying informed,
we collectively contribute to advancing diabetes care
and enhancing the lives of those affected by this condition.
[Download the Closed-Loop Systems Overview Here]
Kind regards,




